GM Blog of a 40 yr old male patient
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and prognosis
A 40 year old male resident of athmakur daily wageworker by occupation came to the OPD with the chief complaints of
CHIEF COMPLAINTS:
Complaints of swelling of face since 1 month
Compliants of lesions in the mouth since 1 month
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic 24 years back then he started taking toddy and then gradually shifted to take whiskey in next 6 months. Currently consuming 9 units per day (90ml) since the last 4 months. Patient has strong urge to take alcohol on waking up.he experiences increased sweating, tremors,sleep disturbances, restlessness and hearing voices when stopped consuming alcohol.he continues to take alcohol despite knowing it's harmful effects. Patient started smoking tobacco since last 5 years.experiences irritability and headache when tobacco is stopped. He continues to smoke despite knowing it's harmful effects.
No history of vomiting, loose stools, burning mituration,foul smelling, head injury, palpitations, seizures.
PAST HISTORY
Known case of peptic ulcer disease since 7 years and on medication.
Known case of diabetes mellitus since 2 years and on medication.
History of hallucinations 1 year back after stopping alcohol for 3 days.
Not a known case hypertension,TB, asthma,CHD,CVA, epilepsy, thyroid disorders.
PERSONAL HISTORY :
- Diet: mixed
- Appetite: decreased
- Bowel habits: normal
- Bladder habits: normal
- Sleep: decreased
- No history of allergies.
- Addictions: alcohol consumption Whisky(180ml) daily since 24 years.
- Smoking beedi 10 -12 per day since 5 years.
FAMILY HISTORY : his father is also drunker.
His mother committed suicide 20 years back.
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative, well oriented to time,place and person.
- Pallor - absent
- Icterus - absent
- Clubbing - absent
- Lymphadenopathy - absent
- Cyanosis - absent
- Pedal edema - absent
Patient is c/c/c
Temp:- 97.2 F
PR- 80bpm
BP- 120/80 mm of Hg
Spo2-
GRBS- 320 mg per dl
On abdominal examination:
Inspection:
Shape of abdomen is scaphoid
Flanks are free
Umblicus is in position, everted
Skin over abdomen normal shiny, no scars, no sinuses, no nodules, no puncture marks.
No visible veins.
No engorged veins.
Movements of abdominal wall are normal, no visible gaatric peristalsis
Palpation:
Liver examination:
On superficial palpation
No tenderness , normal temperature
On deep palpation
No tenderness in liver
Non pulsatile
Spleen examination:
No tenderness and pain
Percussion :
Auscultation
CVS Examination :
Inspection :
No abnormal palsations
No visible scars.
No chest deformities.
Mediastinum normal
Trachea central in position.
Palpation :
Mediastinal position : apex beat palpable in 5 th intercostal space.
Position of trachea normal.
Percussion :
Ascultation : on examination of mitral area, pulmonary area, tricuspid area and aortic area S1 and S2 heard. No murmurs heard.
Respiratory system examination :
Mild anterior deviated nasal septum towards left side.
Inspection :
Position of trachea central
No dropping off shoulders
No intercostal indrawing
No supraclavicular hallowness
Shape and symmetry of the chest normal.
No dilated veins.
No visible scars.
accessory muscles of respiration not prominent.
Palpation :
On three finger test : position of the trachea central.
Respiratory movements are normal.
Vocal framitus : on palpation of right and left sides in all the areas vibrations are normal on both sides.
On Percussion :
No cardiomegaly
Ascultation :
Vocal resonence : equal on both sides in all areas
Normal vesicular breath sounds heard.
Bilateral air entry present.
CNS :
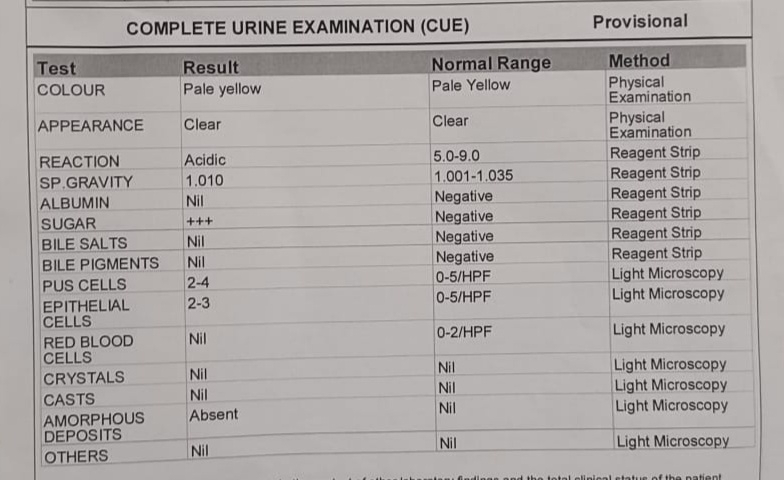
INVESTIGATIONS
Complete blood picture
Random blood sugar
Liver function test
Renal function test
Blood grouping
PROVISIONAL DIAGNOSIS:
Alcohol and tobacco dependence syndrome with type 2 diabetes mellitus.
Treatment










Comments
Post a Comment